Kaletra Side Effects
Generic name: lopinavir / ritonavir
Medically reviewed by Drugs.com. Last updated on Mar 4, 2023.
Note: This document contains side effect information about lopinavir / ritonavir. Some dosage forms listed on this page may not apply to the brand name Kaletra.
Applies to lopinavir / ritonavir: oral solution, oral tablet.
Serious side effects of Kaletra
Along with its needed effects, lopinavir / ritonavir may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking lopinavir / ritonavir:
Less common
- Bloating
- blurred vision
- chills
- constipation
- darkened urine
- dry mouth
- fast heartbeat
- fever
- flushed, dry skin
- fruit-like breath odor
- increased hunger
- increased thirst
- increased urination
- indigestion
- loss of appetite
- loss of consciousness
- nausea
- pains in the stomach, side, or abdomen, possibly moving to the back
- sweating
- troubled breathing
- unexplained weight loss
- vomiting
- yellow eyes or skin
Incidence not known
- Blistering, peeling, or loosening of the skin
- chest pain or discomfort
- cough
- diarrhea
- itching
- joint or muscle pain
- lightheadedness, dizziness, or fainting
- red skin lesions, often with a purple center
- red, irritated eyes
- slow or irregular heartbeat
- sore throat
- sores, ulcers, or white spots in the mouth or on the lips
- unusual tiredness or weakness
Get emergency help immediately if any of the following symptoms of overdose occur while taking lopinavir / ritonavir:
Symptoms of overdose
- Agitation
- confusion
- cool, sweaty skin
- decreased appetite
- decreased awareness or responsiveness
- decreased urine output
- depression
- fast, irregular, or pounding heartbeat
- fast, shallow breathing
- general feeling of discomfort
- headache
- hostility
- irritability
- muscle pain or cramping
- muscle twitching
- pounding, slow heartbeat
- rapid weight gain
- seizures
- severe sleepiness
- stomach discomfort
- swelling of the face, ankles, or hands
- swelling of the feet or lower legs
- unusual drowsiness, dullness, tiredness, weakness, or feeling of sluggishness
Other side effects of Kaletra
Some side effects of lopinavir / ritonavir may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common
- Abnormal stools
- belching
- heartburn
- lack or loss of strength
- pain
- skin rash
- trouble with sleeping
Incidence not known
- Redistribution of body fat
For Healthcare Professionals
Applies to lopinavir / ritonavir: oral capsule, oral liquid, oral tablet.
General
In clinical studies, this drug was used with nucleoside reverse transcriptase inhibitors with or without efavirenz or nevirapine. The most common side effects were diarrhea, nausea, vomiting, hypertriglyceridemia, and hypercholesterolemia. Diarrhea, nausea, and vomiting occurred more often at the start of therapy while hypertriglyceridemia and hypercholesterolemia generally occurred later. Diarrhea was reported more often when this drug was used once a day than when it was used twice a day.[Ref]
Other
Increased total cholesterol (greater than 300 mg/dL) and triglycerides (greater than 750 mg/dL) have been reported in up to 39% and up to 36% of patients, respectively. Decreased inorganic phosphorus (less than 1.5 mg/dL) has been reported in up to 2% of patients.[Ref]
Very common (10% or more): Increased total cholesterol (up to 39%), increased triglycerides (up to 36%)
Common (1% to 10%): Fatigue, asthenia, pain, decreased weight, pyrexia, chills, decreased inorganic phosphorus
Uncommon (0.1% to 1%): Increased weight
Frequency not reported: Generalized pain, back and abdomen enlargement, chest pain, cyst, edema, peripheral edema, face edema, influenza syndrome, hypertrophy, malaise, drug interaction, increased drug level, bacterial infection, viral infection, otitis media, breast enlargement
Antiretroviral therapy:
-Frequency not reported: Increased weight, increased blood lipid levels[Ref]
Hepatic
Very common (10% or more): Increased GGT (up to 29%), increased ALT (up to 11%)
Common (1% to 10%): Increased AST, hepatitis (including increased AST, ALT, GGT), increased total bilirubin
Uncommon (0.1% to 1%): Hepatomegaly, cholangitis, hepatic steatosis, hyperbilirubinemia, jaundice
Frequency not reported: Fatty liver deposit, cytolytic hepatitis, liver tenderness, hepatic failure, cholecystitis, hepatic dysfunction
Postmarketing reports: Jaundice, hepatitis[Ref]
Increased GGT (greater than 300 units/L), ALT (greater than 215 units/L), AST (greater than 180 units/L), and total bilirubin (greater than 3.48 mg/dL) have been reported in up to 29%, up to 11%, up to 10%, and 1% of patients, respectively.
Patients with underlying hepatitis B or C or marked elevations in transaminases before initiation of therapy may be at an increased risk for developing further transaminase elevations or liver decompensation. There have been reports of hepatic dysfunction with some cases leading to death. A causal relationship with this drug has not been proven since these cases have generally occurred in patients with advanced HIV who also had underlying chronic hepatitis or cirrhosis and were taking multiple concomitant medications.[Ref]
Gastrointestinal
Very common (10% or more): Diarrhea (up to 28%), nausea (up to 16%)
Common (1% to 10%): Increased amylase, vomiting, abdominal pain, upper abdominal pain, lower abdominal pain, increased lipase, gastroenteritis and colitis, dyspepsia, pancreatitis, gastroesophageal reflux disease, hemorrhoids, flatulence, abdominal distention, abnormal feces, constipation, dysphagia
Uncommon (0.1% to 1%): Stomatitis and oral ulcers, duodenitis, gastritis, gastrointestinal hemorrhage (including rectal hemorrhage), dry mouth, gastrointestinal ulcer, fecal incontinence
Frequency not reported: Abdominal discomfort, enteritis, enterocolitis, eructation, esophagitis, gastric disorder, gastric ulcer, hemorrhagic enterocolitis, mouth ulceration, periodontitis, sialadenitis, stomach discomfort, ulcerative stomatitis[Ref]
Increased amylase (greater than 2 times the upper limit of normal [2 x ULN]) and lipase (greater than 2 x ULN) were reported in up to 8% and up to 5% of patients, respectively.
Pancreatitis, including fatalities, has occurred in patients receiving this drug, including those who developed hypertriglyceridemia. Although a causal relationship has not been established, marked triglyceride elevation is a risk factor for the development of pancreatitis.[Ref]
Respiratory
Very common (10% or more): Upper respiratory tract infection (up to 13.9%)
Common (1% to 10%): Lower respiratory tract infection, bronchitis
Frequency not reported: Asthma, bronchopneumonia, dyspnea, pulmonary edema, pharyngitis, rhinitis, increased cough, sinusitis, influenza[Ref]
Metabolic
Increased glucose (greater than 250 mg/dL) and uric acid (greater than 12 mg/dL) have each been reported in up to 5% of patients.
Episodes of hyperglycemia, new onset diabetes mellitus, and exacerbation of preexisting diabetes mellitus have been reported during postmarketing studies in HIV-infected patients receiving protease inhibitors. In some cases, diabetic ketoacidosis has occurred. No causal relationship has been established.[Ref]
Common (1% to 10%): Hypercholesterolemia, hypertriglyceridemia, increased glucose, increased uric acid, decreased appetite, blood glucose disorders (including diabetes mellitus), anorexia
Uncommon (0.1% to 1%): Lactic acidosis, increased appetite
Frequency not reported: Avitaminosis, hypovitaminosis, dehydration, dyslipidemia, hyperamylasemia, hyperlipasemia, decreased glucose tolerance, lipomatosis, obesity, hyperglycemia, new onset diabetes mellitus, exacerbation of preexisting diabetes mellitus, ketoacidosis, insulin resistance, hyperlactatemia
Postmarketing reports: Redistribution/accumulation of body fat (including central obesity, dorsocervical fat enlargement, peripheral wasting, facial wasting, breast enlargement, "cushingoid appearance")
Combination antiretroviral therapy:
-Frequency not reported: Redistribution of body fat (fat loss or fat gain)
Antiretroviral therapy:
-Frequency not reported: Redistribution/accumulation of body fat, increased glucose levels[Ref]
Musculoskeletal
Common (1% to 10%): Musculoskeletal pain (including arthralgia, back pain), increased creatine phosphokinase, myalgia, muscle disorders (such as weakness, spasms)
Uncommon (0.1% to 1%): Rhabdomyolysis, osteonecrosis
Frequency not reported: Arthropathy, arthrosis, muscular weakness, joint disorder, osteoarthritis, extremity pain, myasthenia, myositis, perineal abscess[Ref]
Increased creatine phosphokinase (greater than 4 x ULN) was reported in up to 5% of patients.[Ref]
Nervous system
Common (1% to 10%): Headache (including migraine), neuropathy (including peripheral neuropathy), dizziness, paresthesia
Uncommon (0.1% to 1%): Ageusia, convulsion, vertigo, tremor, cerebrovascular accident/event, tinnitus, dysgeusia
Frequency not reported: Amnesia, ataxia, balance disorder, abnormal coordination, cerebral infarction, dyskinesia, encephalopathy, facial paralysis/palsy, hypertonia, peripheral neuritis, somnolence, hyperacusis, extrapyramidal disorder[Ref]
Hematologic
Decreased neutrophils (less than 0.75 x 10[9]/L) and hemoglobin (less than 8 g/dL) have been reported in up to 5% and up to 2% of patients, respectively.[Ref]
Common (1% to 10%): Decreased neutrophils, anemia, decreased hemoglobin, leukopenia, neutropenia, lymphadenopathy
Rare (less than 0.1%): Hemolytic anemia, spontaneous bleeding in hemophiliacs
Frequency not reported: Splenomegaly[Ref]
Psychiatric
Common (1% to 10%): Anxiety, insomnia, decreased libido, depression
Uncommon (0.1% to 1%): Abnormal dreams
Frequency not reported: Affect lability, agitation, apathy, confusional state, disorientation, mood swings, nervousness, abnormal thinking[Ref]
Dermatologic
Common (1% to 10%): Rash (including maculopapular rash), skin infections (including cellulitis, folliculitis, furuncle), acquired lipodystrophy (including facial wasting), dermatitis/rash (including eczema, seborrheic dermatitis), night sweats, pruritus
Uncommon (0.1% to 1%): Alopecia, capillaritis, vasculitis
Rare (0.01% to 0.1%): Stevens-Johnson syndrome, erythema multiforme
Frequency not reported: Acne, dry skin, acneiform dermatitis, allergic dermatitis, exfoliative dermatitis, idiopathic capillaritis, generalized rash, nail disorder, seborrhea, benign skin neoplasm, skin discoloration, skin hypertrophy, skin ulcer, skin striae, swelling face, hyperhidrosis, acute generalized exanthematous pustulosis, furunculosis
Postmarketing reports: Toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme[Ref]
Renal
Common (1% to 10%): Decreased calculated CrCl, renal failure
Uncommon (0.1% to 1%): Nephritis
Frequency not reported: Nephrolithiasis, renal disorder
Postmarketing reports: Nephrolithiasis[Ref]
Decreased calculated CrCl (less than 50 mL/min) was reported in up to 3% of patients.[Ref]
Hypersensitivity
Common (1% to 10%): Hypersensitivity (including urticaria, angioedema)
Frequency not reported: Drug hypersensitivity, severe skin and mucous hypersensitivity reaction with transient multiorgan failure[Ref]
Cardiovascular
Common (1% to 10%): Hypertension, vasodilatation
Uncommon (0.1% to 1%): Deep vein thrombosis, atherosclerosis (such as myocardial infarction), atrioventricular (AV) block, tricuspid valve incompetence
Frequency not reported: Distended veins, angina pectoris, atrial fibrillation, chest pain, palpitation, orthostatic hypotension, thrombophlebitis, varicose vein, vasculitis, sinus arrest, bradycardia-tachycardia syndrome
Postmarketing reports: Bradyarrhythmias, first-degree AV block, second-degree AV block, third-degree AV block, QTc interval prolongation, torsades de pointes[Ref]
Genitourinary
Common (1% to 10%): Erectile dysfunction, menstrual disorders, amenorrhea, menorrhagia
Uncommon (0.1% to 1%): Hematuria
Frequency not reported: Ejaculation disorder, impotence, abnormal urine odor, urine abnormality[Ref]
Endocrine
Common (1% to 10%): Hypogonadism
Frequency not reported: Cushing's syndrome, hypothyroidism, gynecomastia[Ref]
Ocular
Uncommon (0.1% to 1%): Visual impairment
Frequency not reported: Visual disturbance, eye disorder[Ref]
Immunologic
Uncommon (0.1% to 1%): Immune reconstitution syndrome/immune reconstitution inflammatory syndrome
Frequency not reported: Autoimmune disorders in the setting of immune reconstitution (e.g., Graves' disease, polymyositis, Guillain-Barre syndrome, autoimmune hepatitis)
Oncologic
Frequency not reported: Neoplasm, lipoma
More about Kaletra (lopinavir / ritonavir)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (4)
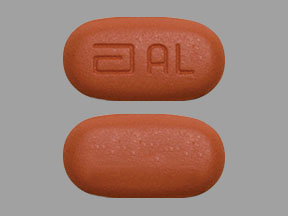
- Drug images
- Dosage information
- During pregnancy
- Generic availability
- Drug class: protease inhibitors
- En español
Patient resources
Professional resources
Related treatment guides
References
1. Product Information. Kaletra (lopinavir-ritonavir). Abbott Pharmaceutical. 2001;PROD.
2. Hicks C, King MS, Gulick RM, et al. Long-term safety and durable antiretroviral activity of lopinavir / ritonavir in treatment-naive patients: 4 year follow-up study. AIDS. 2004;18:775-779.
3. Guest JL, Ruffin C, Tschampa JM, DeSilva KE, Rimland D. Differences in rates of diarrhea in patients with human immunodeficiency virus receiving lopinavir-ritonavir or nelfinavir. Pharmacotherapy. 2004;24:727-35.
4. Cerner Multum, Inc. UK Summary of Product Characteristics.
5. Borras-Blasco J, Belda A, Rosique-Robles D, Castera E, Abad J, Amoros-Quiles I. Hair loss induced by lopinavir-ritonavir. Pharmacotherapy. 2007;27:1215-8.
6. Leon A, Martinez E, Sarasa M, et al. Impact of steady-state lopinavir plasma levels on plasma lipids and body composition after 24 weeks of lopinavir / ritonavir-containing therapy free of thymidine analogues. J Antimicrob Chemother. 2007.
7. Warnke D, Barreto J, Temesgen Z. Antiretroviral drugs. J Clin Pharmacol. 2007;47:1570-9.
8. Cerner Multum, Inc. Australian Product Information.
9. Rabaud C, Burty C, Grandidier M, et al. Tolerability of postexposure prophylaxis with the combination of zidovudine-lamivudine and lopinavir-ritonavir for HIV infection. Clin Infect Dis. 2005;40:303-5.
10. Johnson M, Grinsztejn B, Rodriguez C, et al. 96-week comparison of once-daily atazanavir/ritonavir and twice-daily lopinavir / ritonavir in patients with multiple virologic failures. AIDS. 2006;20:711-718.
11. Cameron DW, Becker S, King MS, et al. Exploratory study comparing the metabolic toxicities of a lopinavir / ritonavir plus saquinavir dual protease inhibitor regimen versus a lopinavir / ritonavir plus zidovudine/lamivudine nucleoside regimen. J Antimicrob Chemother. 2007;59:957-63.
12. Drugs for HIV infection. Treat Guidel Med Lett. 2009;7:11-22.
13. Bongiovanni M, Bini T, Tordato F, et al. Immunovirological outcomes in 70 HIV-1-infected patients who switched to lopinavir / ritonavir after failing at least one protease inhibitor-containing regimen: a retrospective cohort study. J Antimicrob Chemother. 2003;51:171-4.
14. Martinez E, Domingo P, Galindo MJ, et al. Risk of metabolic abnormalities in patients infected with HIV receiving antiretroviral therapy that contains lopinavir-ritonavir. Clin Infect Dis. 2004;38:1017-23.
15. Doco-Lecompte T, Garrec A, Thomas L, Trechot P, May T, Rabaud C. Lopinavir-ritonavir (Kaletra) and lithiasis: seven cases. AIDS. 2004;18:705-6.
16. Canta F, Marrone R, Bonora S, et al. Pharmacokinetics and hepatotoxicity of lopinavir / ritonavir in non-cirrhotic HIV and hepatitis C virus (HCV) co-infected patients. J Antimicrob Chemother. 2005.
17. Johnson M, Grinsztejn B, Rodriguez C, et al. Atazanavir plus ritonavir or saquinavir, and lopinavir / ritonavir in patients experiencing multiple virological failures. AIDS. 2005;19:685-94.
18. Manfredi R, Sabbatani S. Serious, multi-organ hypersensitivity to lopinavir alone, involving cutaneous-mucous rash, and myeloid, liver, and kidney function. AIDS. 2006;20:2399-2400.
19. Soriano V, Puoti M, Sulkowski M, et al. Care of patients coinfected with HIV and hepatitis C virus: 2007 updated recommendations from the HCV-HIV International Panel. AIDS. 2007;21:1073-89.
20. Voigt E, Wasmuth JC, Vogel M, et al. Safety, Efficacy and Development of Resistance under the New Protease Inhibitor Lopinavir/Ritonavir: 48-Week Results. Infection. 2004;32:82-8.
21. Hammer SM, Saag MS, Schechter M, et al. Treatment for adult HIV infection: 2006 recommendations of the International AIDS Society-USA panel. JAMA. 2006;296:827-43.
22. Brennan-Benson P, Pakianathan M, Rice P, et al. Enfurvitide prevents vertical transmission of multidrug-resistant HIV-1 in pregnancy but does not cross the placenta. AIDS. 2006;20:297-9.
23. Molto J, Santos JR, Negredo E, Miranda C, Videla S, Clotet B. Lopinavir / ritonavir monotherapy as a simplification strategy in routine clinical practice. J Antimicrob Chemother. 2007;60:436-9.
24. Roberts DM, Ray JE, Buckley NA. Mild clinical toxicity and dose-dependent pharmacokinetics following acute lopinavir / ritonavir poisoning in a HIV-positive patient. AIDS. 2008;22:792-3.
25. Borras-Blasco J, Navarro-Ruiz A, Borras C, Castera E. Adverse cutaneous reactions associated with the newest antiretroviral drugs in patients with human immunodeficiency virus infection. J Antimicrob Chemother. 2008;62:879-88.
26. Badiou S, De Boever CM, Dupuy AM, Baillat V, Cristol JP, Reynes J. Small dense LDL and atherogenic lipid profile in HIV-positive adults: influence of lopinavir / ritonavir-containing regimen. AIDS. 2003;17:772-4.
27. Bergersen BM. Cardiovascular Risk in Patients with HIV Infection : Impact of Antiretroviral Therapy. Drugs. 2006;66:1971-87.
28. Yazdanpanah Y, Viget N, Cheret A, et al. Increased bleeding in HIV-positive haemophiliac patients treated with lopinavir-ritonavir. AIDS. 2003;17:2397-9.
29. Ghosn J, Duvivier C, Tubiana R, Katlama C, Caumes E. Acute generalized exanthematous pustulosis induced by HIV postexposure prophylaxis with lopinavir-ritonavir. Clin Infect Dis. 2005;41:1360-1.
30. Yotsumoto M, Kitano K, Saito H. Bradycardia-tachycardia syndrome induced by lopinavir-ritonavir in a patient with AIDS. AIDS. 2005;19:1547-8.
31. Worm SW, Sabin C, Weber R, et al. Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: The Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) Study. J Infect Dis. 2009;201:318-30.
32. Calza L, Manfredi R, Verucchi G. Myocardial infarction risk in HIV-infected patients: epidemiology, pathogenesis, and clinical management. AIDS. 2010;24:789-802.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.